
How Gut Microbes Reduce Intestinal Inflammation
Beneficial gut microbes are considered as healthy, having an influence on brain health and overall immune functioning, however many haven’t considered how gut microbes could influence intestinal inflammation. Intestinal inflammation is becoming more and more of a health issue globally. There is a growing number of sufferers from gut inflammatory diseases such as IBS, Crohn’s disease and Coeliacs disease.
Central to gut inflammation is oxidative stress and the highly inflammatory nature of many western diets is a possible driver for this increase. Many diets lack essential nutrients, antioxidants or are not good for beneficial gut microbes. Gut microbes play a key but unappreciated role in managing inflammation within the gut. The full spectrum of their role is being assessed by gut microbe researchers.
In this article we will consider the latest research on how gut microbes could influence intestinal inflammation. Specifically, how beneficial gut microbes may reduce intestinal inflammation and encourage better outcomes for sufferers of gut inflammation.
Intestinal Inflammation
Inflammation within the gut can occur with the build up of oxidative stresses in intestinal cells or from additional immune system overactivation in the gut.
Intestinal oxidative stress happens when highly reactive radical molecules and intestinal cell damage outweighs body antioxidants, or intestinal repair responses. This worsens any pre-existing intestinal cell damage, initiating inflammation and immune cells as a defence response. Of course, with chronic oxidative stress, from a poor diet for example, this inflammation can become chronic.
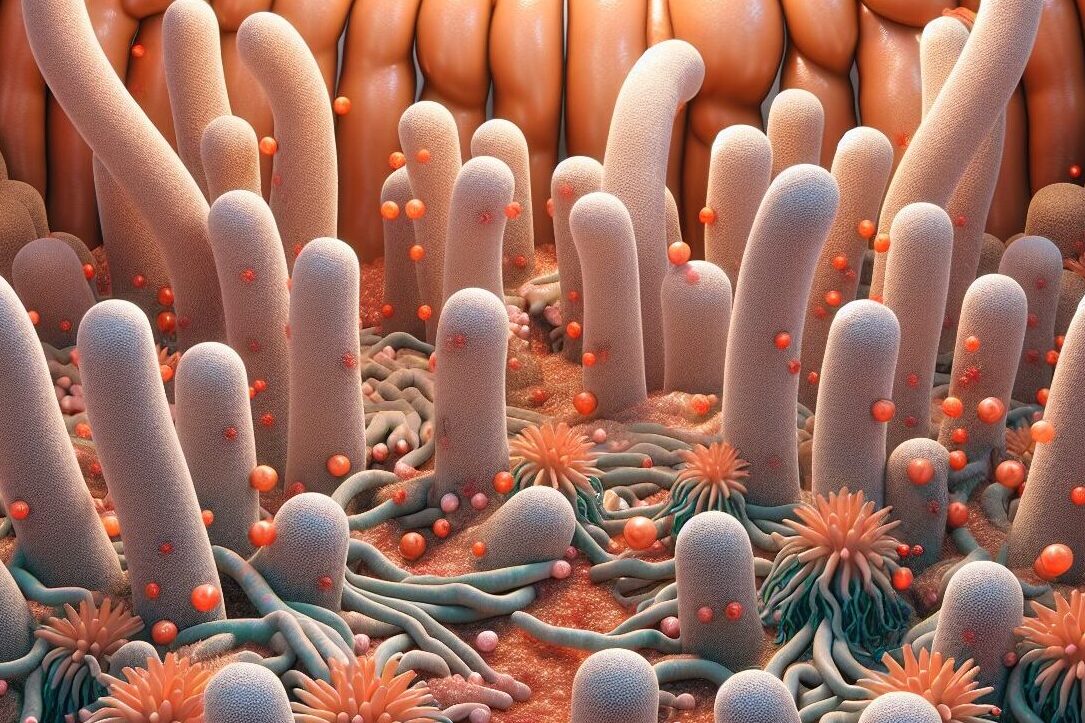
The gastrointestinal tract is lined with cells that are vulnerable to pathogens and harmful proteins. When the immune response from these intestinal cells is activated excessively, inflammatory pathways are also triggered.
If gut inflammatory pathways are constantly activated, gut inflammatory pathologies such as IBS and Crohn’s disease can also develop alongside this. You see a runaway gut inflammatory response within the body. Symptoms of gut inflammation are abdominal pains, diarrhoea, fatigue and malnutrition. If gut inflammation is allowed to progress even further, with very chronic inflammation, one can develop colorectal cancers or intestinal strictures.
Malnutrition may seem like an odd symptom from inflammation. You may be wondering how those outcomes can be linked. Essentially, when intestinal cells are constantly inflamed and are unable to recover to normal cell numbers they are less able to help with nutrient absorption. The functioning of the intestinal barrier is disrupted with chronic gut immunoinflammation, worsening gut tissue damage and gut functioning.
This is why you see Coeliac disease pathologies, with less optimal nutrient intake. You can measure this change in nutrient levels, resulting from excessive gut inflammation, via a blood test. That is also why suffers of gut inflammation can experience fatigue. This is a key reason why encouraging a healthy gut and minimal gut inflammation is important for our overall wellbeing.

Gut Microbes And Gut Inflammation
Our gut microbes can play a role in influencing levels of inflammation in the gut. Pathogenic microbes can do this through activating the immune system and invading our intestinal cells, making levels of gut inflammation worse. Through these actions these bad, or pathogenic, microbes can cause gut oxidative stress levels to rise. Which is why they make gut inflammation worse.
On the other hand, there are beneficial gut microbes that live in our gut and positively contribute to our health. The body recognises these microbes as beneficial and they are non-invasive of gut tissues. This means they don’t trigger our inflammatory and immune system responses within the gut. In fact, they are actually able to reduce levels of inflammation in the gut. Beneficial gut microbes also offer a level of microbial competition. That prevents pathogenic bacteria from being able to settle in the intestines and cause inflammatory damage.
The relationships between beneficial gut microbes and ourselves have ancient ancestral origins. Antioxidants from beneficial gut microbes are thought to have a massive influence on gut oxidative stress levels and inflammation. Gut microbe antioxidants, from our set of beneficial gut microbes, help them to survive in our gut. They also seem to be of benefit to us and levels of inflammatory responses.
Beneficial gut microbes produce SCFAs, polysaccharides, antioxidant enzymes and tryptophan molecules. Certain microbes produce these compounds at better levels than others. They are anti-inflammatory and antioxidant molecules, exhibiting effects on our gut at very small level. There are many recent studies showing how they are preventative on the gut dysbiosis and oxidative stress that leads to inflammatory gut diseases.
Researched Anti-Inflammatory Effects Of Beneficial Gut Microbes
Because of how unknown this field was only ten years ago, there has been an explosive amount of research into beneficial gut microbes. At first anti-inflammatory gut effects were not even recognised. However, with extensive research, factors like intestinal permeability, gut microbe antioxidants and fatty acid molecules became widely recognized factors in managing our gut health.
Intestinal Permeability
Studies with beneficial gut microbes have found that SCFAs, or free short fatty acids, made by microbes improve intestinal barrier function. When the gut is more permeable to the contents of the gut, inflammatory disease-causing pathogens, damaging toxins and proteins can enter.
Expression of intestinal genes coding for closing off intestinal permeability to foreign pathogens are improved with SCFAs from beneficial gut microbes. Some of these intestinal proteins are occluding and ZO-1, these help to seal off intestinal cells.
The overall effect of that activity is anti-inflammatory, as measured by reduced levels of inflammatory cytokines and reactive oxygen molecules in the gut. This reduction in inflammation is because less inflammatory causing molecules can disrupt the intestinal cells.
SCFAs
Supplementing with microbial SCFAs also encouraged a healthier gut microbe composition, while improving intestinal barrier function. Research also shows that improving levels of gut microbes that make SCFAs may improve the response of the gut to IBD treatments.
Supplementation with SCFAs also improved levels of antioxidant enzymes, such as glutathione peroxidase, which are important for managing inflammation. SCFAs may reverse fatty acid peroxidation in the gut too, which is a huge source of oxidative stress and inflammation. Research shows probiotic microorganisms, that produce molecules like SCFAs, positively affect intestinal inflammatory signalling pathways.

Butyrate And Inflammatory Signalling
Butyrate is one molecule made by beneficial gut microbes that is also thought to help with reducing gut inflammation. It managed to significantly reduce colitis in one study, encouraging a anti-inflammatory gut cell response. This included lowered levels of inflammatory signalling molecules known as IL-6 and IL-12. Butyrate seems to help to reduce intestinal immune responses, with this action mediated through those inflammatory lowering signalling pathways.
Butyrate also managed to reduce some symptoms of IBD in a study patients suffering with IBD. This compound was identified as being able to encourage intestinal cell repair, while it may also encourage more beneficial gut bacteria to grow in the gut.

Microbial Antioxidants
SCFAs and butyrate are examples of microbial specific compounds that we are currently aware of. There are interesting antioxidant compounds known to be produced by gut bacteria, like melatonin, that may have an influence on our gut health. Research with postbiotics suggests that there could also be other anti-inflammatory molecules from beneficial gut microbes that research is currently not aware of.
Some of these may be antioxidant molecules, like some of those detected in strains of notorious beneficial gut microbes Lactobacillus and Bifidobacterium. Antioxidant and anti-inflammatory signalling has been observed in probiotic strains of these beneficial gut microbes.
Microbial antioxidants seem to encourage more beneficial gut microbes to grow too. In this way they recruit more beneficial gut microbes, encouraging optimal gut microbe diversity, reducing gut pathogens and further lowering gut inflammation.
There may also be an interaction between gut microbe antioxidants and our intestinal lining mitochondria. With gut microbes reducing oxidative stress from our energy producing mitochondria. This lowers gut inflammation and could improve our overall gut health.
Microbial Exopolysaccharides Or EPS
Exopolysaccharides are just small units of sugar molecules bound together that are made by beneficial gut microorganisms. Lactobacillus helveticus is a gut bacteria that is known to be a non-invasive bacteria in our intestines. This bacteria seems to produce complex sugars that promote improved antioxidant activities within the gut. These EPS, or microbial exopolysaccharides, molecules protect our intestinal cells through reducing oxidative stress. This seems to improve levels of inflammation in the intestines.
Studies also show that they interact with our immune system. In a complex interaction they improve anti-inflammatory signalling, reducing overall inflammation in the intestines. This could be very significant for maintaining optimal intestinal health. They may also improve gut barrier strength, which produces a positive feedback loop, that further improves anti-inflammatory signals in the gut. These remarkable compounds have only really recently been identified as having an anti-inflammatory effect in the gut.
Summary
Beneficial gut microbes seem to have various influences on our health. They may be able to directly influence intestinal inflammation and reduce symptoms associated with certain gut inflammatory diseases including IBD.
Central to gut inflammation is oxidative stress. The highly inflammatory nature of many western diets is a cause of many intestinal issues. Inflammation in the gut is caused by a build-up of oxidative stresses in intestinal cells and immune system overactivation.
The gastrointestinal tract is lined with cells that are vulnerable to pathogens and harmful proteins. Pathogenic microbes can invade our intestinal cells, causing inflammation and activating the immune system. Beneficial gut microbes positively contribute to our health and they are recognised as non-invasive. They don’t trigger our inflammatory and immune system responses.
Beneficial gut microbes produce SCFAs, polysaccharides, antioxidant enzymes and tryptophan molecules. These may have antioxidant and anti-inflammatory effects within the gut.
SCFAs, or free short fatty acids, made by microbes improve intestinal barrier function. A microbial SCFA supplement also encouraged a healthier gut microbe composition. Research shows probiotic microorganisms, that produce SCFAs, reduce intestinal inflammation signals.
Butyrate is a molecule made by beneficial gut microbes which is thought reduce gut inflammation. It may reduce intestinal immune responses and encourage intestinal cell repair.
Microbial antioxidants, made by beneficial gut microbes, encourage more beneficial gut microbes to grow and reduce gut inflammation. Gut microbe antioxidants and our intestinal mitochondria may interact, lowering gut inflammation.
Exopolysaccharides are made by gut bacteria. They can also reduce oxidative stress through immune system interactions and improve gut barrier strength.
Beneficial gut microbes clearly can help to reduce overall levels of inflammation in the gut, supporting optimal gut health.
For more interesting articles, see the main articles page below.





